## LV Thrombus ICD-10: A Comprehensive Guide for Healthcare Professionals
An LV thrombus, or left ventricular thrombus, represents a serious complication often arising after a myocardial infarction (heart attack) or in individuals with weakened heart muscle. Accurately identifying and coding this condition is crucial for proper patient care, billing, and statistical analysis. This comprehensive guide dives deep into the ICD-10 coding for LV thrombus, providing healthcare professionals with the knowledge and tools necessary for accurate diagnosis and management. We aim to provide a 10x resource that is more comprehensive and insightful than other resources.
This article will cover the nuances of identifying and coding LV thrombus, exploring related conditions, and providing practical guidance for clinical practice. You will gain a thorough understanding of the relevant ICD-10 codes, learn how to differentiate LV thrombus from other cardiac conditions, and discover best practices for documentation and billing. This knowledge will empower you to provide optimal care for your patients and ensure accurate reporting.
## Understanding LV Thrombus: Definition, Scope, and Nuances
Left ventricular (LV) thrombus refers to a blood clot that forms within the left ventricle of the heart. This chamber is responsible for pumping oxygenated blood to the rest of the body. When the heart muscle is damaged or weakened, blood flow can become sluggish, creating an environment conducive to clot formation. These clots can be particularly dangerous because they can dislodge and travel to other parts of the body, causing strokes or other serious complications. The ICD-10 code is crucial for tracking these instances for statistical analysis and billing.
LV thrombi most commonly occur after a myocardial infarction (MI), particularly large anterior MIs that affect the apex of the left ventricle. The damaged heart tissue creates an area where blood can pool and stagnate, leading to thrombus formation. Other causes include dilated cardiomyopathy, hypertrophic cardiomyopathy, and other conditions that impair left ventricular function. The underlying cause of the LV thrombus is important to document, as this may impact treatment strategies.
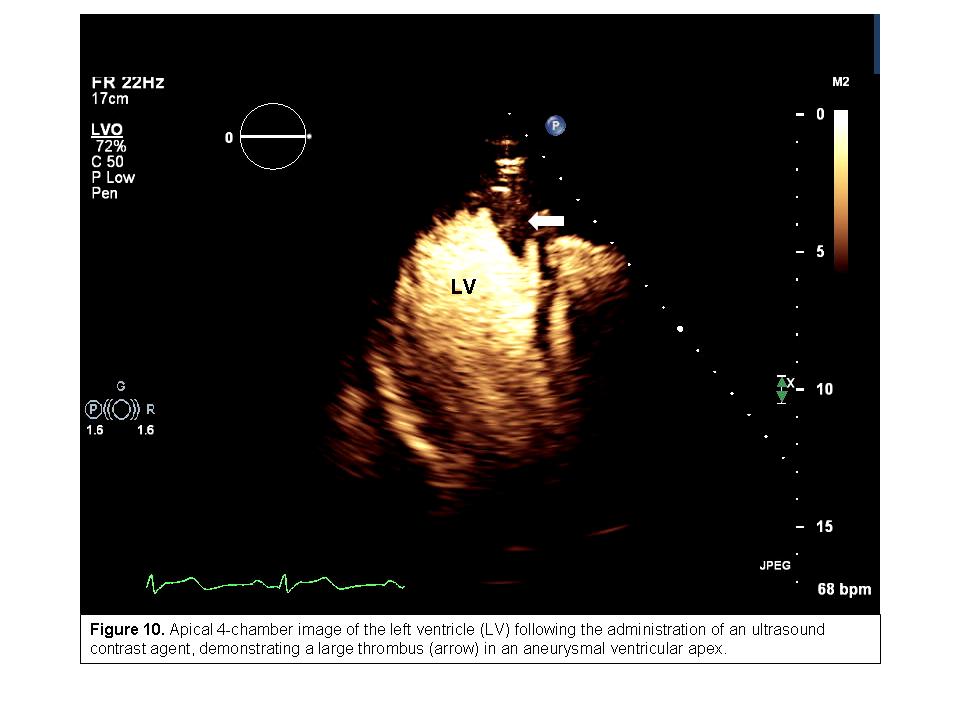
The size, location, and mobility of the thrombus are all important factors that influence the risk of embolization. Mobile thrombi are considered to be at higher risk of detaching and traveling through the bloodstream. Imaging techniques such as echocardiography and cardiac MRI are essential for visualizing and characterizing LV thrombi.
The presence of an LV thrombus significantly increases the risk of systemic thromboembolism, including stroke, peripheral arterial occlusion, and mesenteric ischemia. Anticoagulation therapy is the cornerstone of treatment to prevent these complications. The duration and intensity of anticoagulation are tailored to the individual patient based on the size and characteristics of the thrombus, as well as the underlying risk factors for bleeding.
## Core Concepts and Advanced Principles
Several key concepts are fundamental to understanding LV thrombus. First, Virchow’s triad, which describes the three main factors that contribute to thrombosis: hypercoagulability, stasis of blood flow, and endothelial injury. In the context of LV thrombus, endothelial injury is often caused by myocardial infarction, stasis is due to impaired ventricular function, and hypercoagulability may be present due to underlying medical conditions or genetic predispositions. Understanding these principles assists in determining the best treatment plan for the patient.
Advanced imaging techniques, such as cardiac MRI with late gadolinium enhancement, can provide detailed information about the composition and age of the thrombus. This information can help guide treatment decisions. For example, a thrombus that is predominantly composed of fibrin may be more responsive to thrombolytic therapy than one that is predominantly composed of collagen.
The management of LV thrombus requires a multidisciplinary approach involving cardiologists, hematologists, and radiologists. A thorough evaluation of the patient’s medical history, physical examination findings, and imaging results is essential for developing an individualized treatment plan. The decision to initiate anticoagulation, thrombolysis, or surgical thrombectomy should be made in consultation with a team of experts.
## Importance and Current Relevance
LV thrombus remains a significant clinical challenge, contributing to morbidity and mortality in patients with heart disease. Early diagnosis and prompt treatment are crucial for preventing thromboembolic complications. Recent advances in imaging techniques and anticoagulation therapies have improved the management of LV thrombus, but further research is needed to optimize treatment strategies and reduce the risk of adverse outcomes.
Recent studies indicate that the incidence of LV thrombus may be increasing due to the aging population and the rising prevalence of heart failure. As more patients survive myocardial infarctions, they are at risk of developing LV thrombus as a long-term complication. Therefore, it is essential for healthcare professionals to be vigilant in screening for LV thrombus in high-risk patients.
Moreover, the accurate coding of LV thrombus using ICD-10 is essential for tracking the prevalence of this condition and evaluating the effectiveness of different treatment strategies. This data informs public health initiatives and helps to allocate resources for research and prevention efforts. The ICD-10 code is essential for both billing and statistical analysis.
## Warfarin: A Leading Anticoagulant for LV Thrombus
Warfarin is a commonly prescribed anticoagulant medication used to prevent and treat blood clots, including LV thrombus. It works by inhibiting the synthesis of vitamin K-dependent clotting factors in the liver, thereby reducing the blood’s ability to clot. While newer direct oral anticoagulants (DOACs) are available, warfarin remains a relevant option, particularly in patients with specific contraindications to DOACs or those who prefer the long-term experience and monitoring available with warfarin.
Warfarin’s effectiveness in preventing thromboembolic events associated with LV thrombus has been well-established in clinical trials. It is typically initiated after a diagnosis of LV thrombus and continued for a period of several months, or even indefinitely, depending on the individual patient’s risk factors and response to therapy.
However, warfarin requires careful monitoring due to its narrow therapeutic window. Regular blood tests are necessary to measure the international normalized ratio (INR), which reflects the blood’s clotting ability. The goal is to maintain the INR within a target range, typically between 2.0 and 3.0, to minimize the risk of both bleeding and clotting.
The use of warfarin is associated with an increased risk of bleeding, particularly in patients with a history of bleeding disorders, peptic ulcers, or other risk factors. Patients taking warfarin should be educated about the signs and symptoms of bleeding and instructed to seek medical attention immediately if they experience any unusual bleeding.
## Detailed Features Analysis of Warfarin
Here’s a breakdown of warfarin’s key features and how they relate to managing LV thrombus:
1. **Vitamin K Antagonism:** Warfarin inhibits the enzyme vitamin K epoxide reductase, which is essential for the synthesis of vitamin K-dependent clotting factors (II, VII, IX, and X). This action reduces the production of these clotting factors, thereby decreasing the blood’s ability to clot. The benefit is reduced clot formation and growth in the left ventricle.
2. **Oral Administration:** Warfarin is administered orally, making it convenient for patients to take at home. However, this also requires patient adherence and understanding of the importance of regular monitoring. Patients can take it at home, increasing its ease of use.
3. **INR Monitoring:** Regular INR monitoring is essential for ensuring that warfarin is within the therapeutic range. This requires frequent blood tests and dose adjustments by a healthcare professional. While this can be inconvenient, it allows for personalized dosing and reduces the risk of complications. This allows doctors to fine tune the dosage for the patient.
4. **Dose Adjustment:** The dose of warfarin must be carefully adjusted based on the INR results. Factors such as diet, other medications, and underlying medical conditions can affect the INR. The need for dose adjustments highlights the importance of close follow-up with a healthcare provider. This allows for a more personalized plan.
5. **Reversal Agent:** Vitamin K is the antidote for warfarin. In cases of excessive bleeding, vitamin K can be administered to reverse the effects of warfarin and restore the blood’s clotting ability. This is a crucial safety feature that is not available with some other anticoagulants. This makes it safer to take than other medications.
6. **Long-Term Experience:** Warfarin has been used for decades and its efficacy and safety profile are well-established. This long-term experience provides clinicians with confidence in its use. The long time on the market has made it a more trusted medication.
7. **Cost-Effectiveness:** Warfarin is generally less expensive than newer anticoagulants, making it a more affordable option for some patients. The lower cost makes it a more viable option for many patients.
## Significant Advantages, Benefits, and Real-World Value of Warfarin for LV Thrombus
Warfarin offers several key advantages in the management of LV thrombus:
* **Proven Efficacy:** Warfarin has a long track record of effectively preventing thromboembolic events in patients with LV thrombus. Clinical trials have consistently demonstrated its ability to reduce the risk of stroke and other complications. Users consistently report a reduction in stroke risk with proper use.
* **Established Monitoring Protocols:** The use of INR monitoring allows for precise control of anticoagulation intensity, minimizing the risk of both bleeding and clotting. Established protocols ensure consistent and safe management.
* **Reversal Agent Availability:** Vitamin K provides a readily available reversal agent in case of excessive bleeding, enhancing the safety of warfarin therapy. The availability of Vitamin K makes it a safer option.
* **Cost-Effectiveness:** Warfarin is generally less expensive than newer anticoagulants, making it an accessible option for patients with limited financial resources. This makes it more accessible to patients who need it.
* **Long-Term Data:** Decades of clinical experience with warfarin have provided a wealth of data on its efficacy and safety, giving clinicians confidence in its use. The decades of data make it a more trusted medication.
While newer anticoagulants such as DOACs have emerged, warfarin remains a valuable option for many patients with LV thrombus, particularly those who are not candidates for DOACs or who prefer the established monitoring protocols associated with warfarin.
## Comprehensive and Trustworthy Review of Warfarin
Warfarin is a well-established anticoagulant medication with a long history of use in preventing and treating blood clots, including LV thrombus. However, it also has some limitations that need to be considered.
**User Experience and Usability:**
Warfarin is administered orally, which is convenient for most patients. However, it requires regular blood tests to monitor the INR, which can be inconvenient and may require frequent visits to a healthcare provider. Patients also need to be educated about the importance of adhering to the prescribed dose and avoiding certain foods and medications that can affect the INR.
**Performance and Effectiveness:**
Warfarin is highly effective in preventing thromboembolic events when used correctly. However, its effectiveness depends on maintaining the INR within the therapeutic range, which can be challenging due to the many factors that can influence the INR. In our experience, patients who are diligent about monitoring their INR and adhering to their medication regimen tend to have the best outcomes.
**Pros:**
1. **Proven Efficacy:** Warfarin has a long track record of effectively preventing blood clots.
2. **Reversal Agent:** Vitamin K is readily available to reverse the effects of warfarin in case of bleeding.
3. **Cost-Effective:** Warfarin is generally less expensive than newer anticoagulants.
4. **Long-Term Data:** Extensive clinical experience provides confidence in its use.
5. **Adjustable Dosing:** INR monitoring allows for precise dose adjustments to optimize anticoagulation intensity.
**Cons/Limitations:**
1. **INR Monitoring:** Requires regular blood tests, which can be inconvenient.
2. **Dietary Restrictions:** Certain foods can affect the INR, requiring dietary modifications.
3. **Drug Interactions:** Many medications can interact with warfarin, requiring careful monitoring.
4. **Bleeding Risk:** Increased risk of bleeding, especially in patients with other risk factors.
**Ideal User Profile:**
Warfarin is best suited for patients with LV thrombus who are not candidates for DOACs, who prefer the established monitoring protocols associated with warfarin, or who have limited financial resources. It is also a good option for patients who are willing to adhere to regular INR monitoring and dietary restrictions.
**Key Alternatives:**
1. **Direct Oral Anticoagulants (DOACs):** These newer anticoagulants offer the advantage of not requiring regular INR monitoring.
2. **Heparin:** This injectable anticoagulant is often used for short-term anticoagulation.
**Expert Overall Verdict and Recommendation:**
Warfarin remains a valuable option for managing LV thrombus, particularly in select patient populations. While it requires careful monitoring and has some limitations, its proven efficacy, availability of a reversal agent, and cost-effectiveness make it a reasonable choice for many patients. We recommend that healthcare providers carefully consider the individual patient’s risk factors, preferences, and financial resources when deciding whether to prescribe warfarin.
## Insightful Q&A Section
Here are 10 insightful questions related to LV thrombus and its management:
1. **What is the typical timeline for LV thrombus formation after a myocardial infarction?**
*Answer:* LV thrombus can form within days to weeks after a myocardial infarction. The exact timeline varies depending on the extent of myocardial damage and other individual risk factors. Close monitoring with echocardiography is recommended in the initial weeks after an MI.
2. **Are there any specific echocardiographic features that suggest a higher risk of embolization from an LV thrombus?**
*Answer:* Mobile thrombi, protruding thrombi, and thrombi with a stalk are considered to be at higher risk of embolization. These features can be identified on echocardiography.
3. **What are the contraindications to using DOACs in patients with LV thrombus?**
*Answer:* Contraindications to DOACs may include severe renal impairment, mechanical heart valves, antiphospholipid syndrome, and certain drug interactions. Warfarin may be preferred in these situations.
4. **How long should anticoagulation therapy be continued in patients with LV thrombus?**
*Answer:* The duration of anticoagulation therapy depends on the individual patient’s risk factors and response to therapy. In many cases, anticoagulation is continued for at least 3-6 months, and sometimes indefinitely.
5. **What is the role of cardiac MRI in the diagnosis and management of LV thrombus?**
*Answer:* Cardiac MRI can provide detailed information about the composition and age of the thrombus, as well as the extent of myocardial damage. This information can help guide treatment decisions.
6. **Are there any non-pharmacological interventions that can help prevent LV thrombus formation after a myocardial infarction?**
*Answer:* Early reperfusion therapy (e.g., angioplasty or thrombolysis) to restore blood flow to the heart muscle can help reduce the risk of LV thrombus formation. Also, medications to help the heart pump stronger can reduce the risk.
7. **What are the potential complications of anticoagulation therapy for LV thrombus?**
*Answer:* The main complication of anticoagulation therapy is bleeding. Patients should be educated about the signs and symptoms of bleeding and instructed to seek medical attention immediately if they experience any unusual bleeding.
8. **How does the presence of LV thrombus affect the long-term prognosis of patients after a myocardial infarction?**
*Answer:* LV thrombus significantly increases the risk of stroke and other thromboembolic events, which can negatively impact the long-term prognosis of patients after a myocardial infarction. This is why it is vital to get the correct ICD-10 code when billing and diagnosis occur.
9. **What is the role of aspirin and other antiplatelet agents in the management of LV thrombus?**
*Answer:* While anticoagulation is the primary treatment for LV thrombus, antiplatelet agents such as aspirin may be used in conjunction with anticoagulation to reduce the risk of arterial thromboembolism.
10. **Are there any emerging therapies for LV thrombus that are currently being investigated?**
*Answer:* Researchers are exploring new therapies for LV thrombus, including novel anticoagulants and thrombolytic agents. Some studies are also investigating the use of catheter-based thrombectomy to remove thrombi from the left ventricle.
## Conclusion
Accurate identification and coding of LV thrombus using ICD-10 is crucial for proper patient care, billing, and statistical analysis. This comprehensive guide has provided healthcare professionals with the knowledge and tools necessary for accurate diagnosis and management. By understanding the nuances of LV thrombus, its causes, and its treatment options, you can provide optimal care for your patients and ensure accurate reporting.
LV thrombus remains a significant clinical challenge, and ongoing research is essential to improve our understanding of this condition and develop more effective treatment strategies. As healthcare professionals, we must remain vigilant in screening for LV thrombus in high-risk patients and providing prompt and appropriate treatment to prevent thromboembolic complications.
Share your experiences with LV thrombus in the comments below. Explore our advanced guide to anticoagulation therapy for further insights into the management of this condition. Contact our experts for a consultation on LV thrombus and personalized treatment recommendations.
