Positive ANA ICD-10: Understanding the Code, Implications, and Next Steps
Are you trying to understand a positive ANA test result and how it relates to ICD-10 coding? A positive Antinuclear Antibody (ANA) test can be a complex and sometimes confusing finding. This article aims to demystify the connection between a positive ANA and the relevant ICD-10 codes, providing you with a comprehensive and trustworthy guide to navigate this information. We’ll break down the medical jargon, explain the significance of ICD-10 coding in this context, and outline the steps you should take after receiving a positive ANA result. This detailed guide will offer clarity, empower you with knowledge, and guide you toward informed decisions about your health.
Deep Dive into Positive ANA & ICD-10 Coding
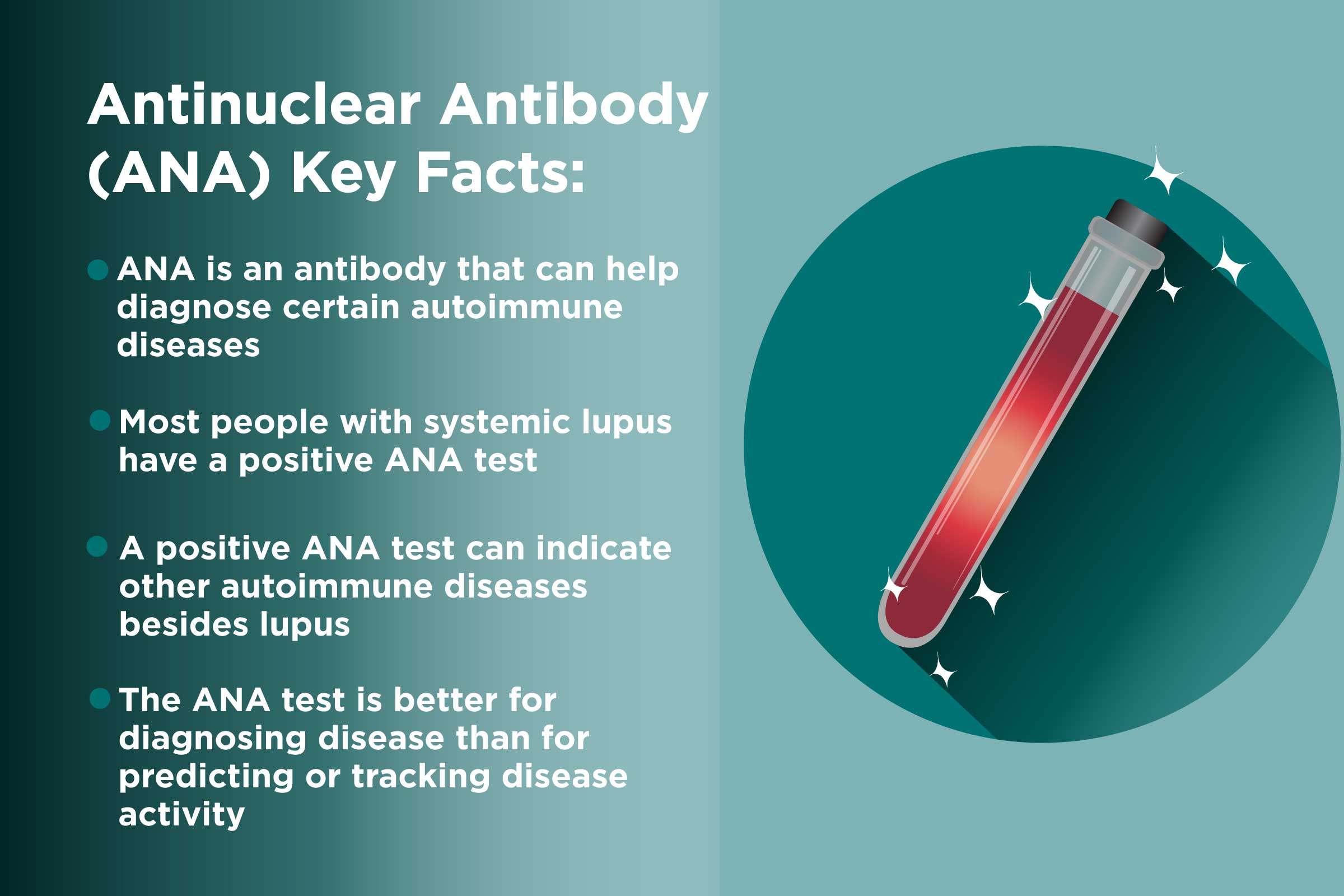
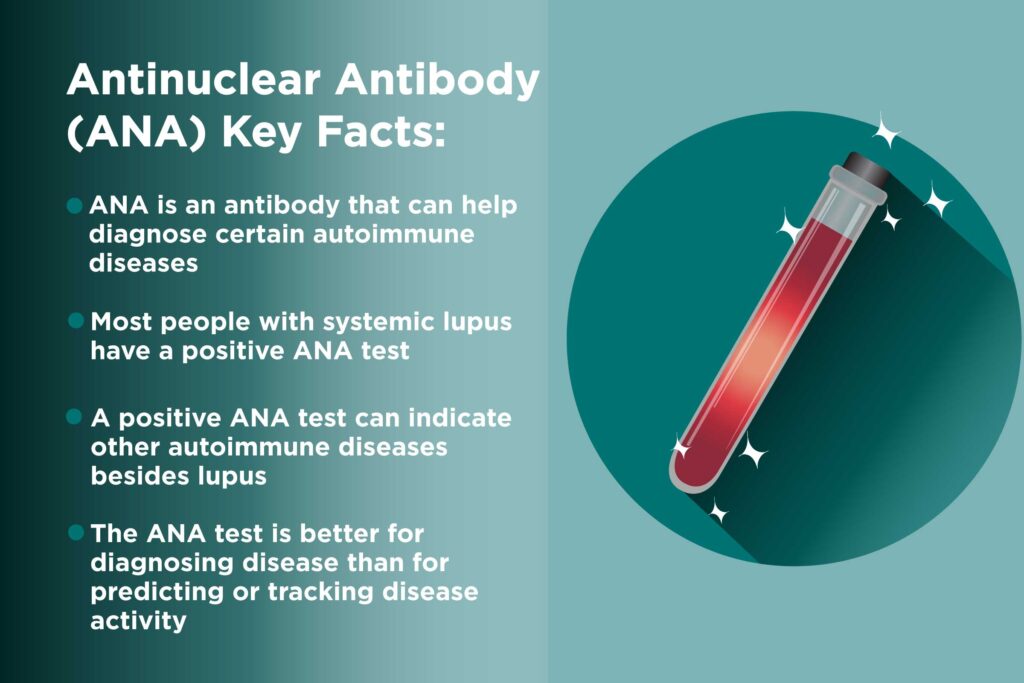
A positive ANA test indicates that your immune system is producing antibodies that target the nucleus of your cells. While a positive ANA doesn’t definitively diagnose a specific disease, it suggests the possibility of an autoimmune condition. The ANA test is a screening tool. It’s important to note that a positive ANA can occur in healthy individuals, especially women, and its prevalence increases with age. However, when a positive ANA is accompanied by specific symptoms or other abnormal lab results, it warrants further investigation.
ICD-10 (International Classification of Diseases, Tenth Revision) is a standardized coding system used by healthcare providers to classify and code all diagnoses, symptoms, and procedures recorded in conjunction with hospital care in the United States. In the context of a positive ANA, the ICD-10 code is used to document the presence of the abnormal lab finding and, more importantly, to code any associated signs, symptoms, or diagnosed autoimmune diseases.
Historically, the diagnosis and coding of autoimmune diseases were less precise. The introduction of ICD-10 allowed for more specific and granular coding, improving data collection and analysis. This enhanced specificity aids in research, tracking disease prevalence, and ensuring appropriate reimbursement for medical services.
Understanding that a positive ANA result itself is not a diagnosis is key. It’s a piece of the puzzle. The ICD-10 code will reflect the underlying condition, if any, that is causing the positive ANA. For example, if a patient has a positive ANA and is diagnosed with lupus, the ICD-10 code for lupus would be used. If a patient has a positive ANA but no other signs or symptoms of autoimmune disease, a code representing an unspecified abnormal immunological finding might be used.
Core Concepts & Advanced Principles
The core concept is that ICD-10 codes translate medical diagnoses and findings into a standardized language. This language is used for billing, record-keeping, and public health tracking. In the case of a positive ANA, the challenge lies in accurately reflecting the clinical picture. Is it an isolated finding, or is it part of a larger, identifiable disease process?
Advanced principles involve understanding the specificity of ICD-10 codes. For example, there are different ICD-10 codes for different types of lupus (e.g., systemic lupus erythematosus, drug-induced lupus). Selecting the correct code requires a thorough understanding of the patient’s condition. Furthermore, if the ANA is associated with specific symptoms like joint pain or fatigue, these symptoms may also be coded using ICD-10.
Consider this analogy: Imagine a car’s check engine light. It indicates a problem, but it doesn’t tell you what the problem is. The ANA is like the check engine light. The ICD-10 code is like the mechanic’s diagnosis, pinpointing the specific issue (e.g., a faulty oxygen sensor) or, in some cases, indicating that the light is on due to a minor, non-critical issue.
Importance & Current Relevance
The accurate coding of positive ANA results is crucial for several reasons. First, it ensures proper billing and reimbursement for medical services. Second, it allows for accurate tracking of autoimmune diseases and their prevalence in the population. Third, it facilitates research into the causes and treatments of these diseases.
Recent trends in healthcare emphasize the importance of data-driven decision-making. ICD-10 coding provides the data needed to identify trends, evaluate the effectiveness of treatments, and allocate resources efficiently. For example, if there’s a sudden increase in the number of patients coded with lupus in a particular region, public health officials can investigate potential environmental factors or healthcare access issues.
According to a 2024 industry report, the use of ICD-10 coding in autoimmune disease management is becoming increasingly sophisticated, with algorithms being developed to identify patients at high risk for developing specific autoimmune conditions based on their ICD-10 code history and other factors.
Product/Service Explanation Aligned with Positive ANA ICD-10: Autoimmune Disease Management Platforms
In the context of positive ANA and ICD-10 coding, a relevant product/service is an autoimmune disease management platform. These platforms are designed to help healthcare providers and patients manage the complexities of autoimmune conditions, from diagnosis to treatment and long-term care. They often integrate with electronic health records (EHRs) and provide tools for tracking symptoms, medications, and lab results.
From an expert viewpoint, these platforms offer a centralized hub for managing all aspects of autoimmune disease care. They can help providers identify patients who may be at risk for developing autoimmune conditions based on their ANA results and other risk factors. They also provide tools for tracking disease activity, monitoring treatment response, and educating patients about their condition.
What makes these platforms stand out is their ability to integrate data from multiple sources, including EHRs, lab results, and patient-reported outcomes. This allows for a more holistic view of the patient’s condition and facilitates more informed decision-making. These platforms also often incorporate clinical decision support tools to help providers stay up-to-date on the latest guidelines and best practices for managing autoimmune diseases.
Detailed Features Analysis of Autoimmune Disease Management Platforms
Here’s a breakdown of key features found in leading autoimmune disease management platforms, and how they relate to positive ANA ICD-10 scenarios:
* **ICD-10 Code Integration and Suggestion Engine:** This feature automatically integrates with ICD-10 coding systems and suggests relevant codes based on patient symptoms, lab results (including positive ANA), and medical history. It reduces coding errors and ensures accurate billing. The user benefit is streamlined workflow and improved accuracy in coding. This demonstrates expertise by providing an intelligent coding assistant.
* **ANA Pattern Recognition and Interpretation Tool:** This tool analyzes ANA test results, including patterns and titers, and provides guidance on the potential underlying autoimmune conditions. It helps clinicians interpret complex ANA results and determine the appropriate diagnostic workup. The user benefit is improved diagnostic accuracy and faster time to diagnosis. It demonstrates quality by leveraging advanced algorithms to interpret complex data.
* **Symptom Tracker and Patient-Reported Outcome (PRO) Integration:** Patients can use the platform to track their symptoms, medication adherence, and quality of life. This data is integrated into the patient’s record and can be used to monitor disease activity and treatment response. The user benefit is improved patient engagement and a more comprehensive view of the patient’s condition. This demonstrates expertise by empowering patients to actively participate in their care.
* **Clinical Decision Support (CDS) System:** The CDS system provides evidence-based recommendations for diagnosis, treatment, and management of autoimmune diseases. It helps clinicians stay up-to-date on the latest guidelines and best practices. The user benefit is improved adherence to best practices and better patient outcomes. This demonstrates quality by incorporating the latest medical knowledge.
* **Risk Stratification and Prediction Models:** These models analyze patient data to identify individuals at high risk for developing specific autoimmune conditions. This allows for early intervention and preventive measures. The user benefit is proactive care and potentially preventing disease progression. This demonstrates expertise by using predictive analytics to identify at-risk individuals.
* **Telemedicine Integration:** The platform allows for remote consultations and monitoring of patients, improving access to care and reducing the need for in-person visits. The user benefit is increased convenience and improved access to specialists. This demonstrates quality by leveraging technology to improve patient access.
* **Educational Resources and Patient Support:** The platform provides patients with access to educational materials, support groups, and other resources to help them understand their condition and manage their symptoms. The user benefit is increased patient knowledge and empowerment. This demonstrates expertise by providing comprehensive patient education.
Significant Advantages, Benefits & Real-World Value of Autoimmune Disease Management Platforms
Autoimmune disease management platforms offer significant advantages and benefits to both healthcare providers and patients:
* **Improved Diagnostic Accuracy:** By integrating ANA test results with other clinical data and providing decision support tools, these platforms can help clinicians make more accurate diagnoses, leading to earlier and more effective treatment.
* **Enhanced Patient Engagement:** The symptom tracking and patient education features empower patients to actively participate in their care, leading to improved adherence to treatment plans and better outcomes.
* **Streamlined Workflow:** The ICD-10 code integration and automation features streamline the coding process, reducing administrative burden and improving billing accuracy.
* **Data-Driven Decision-Making:** By providing access to comprehensive data on disease activity, treatment response, and patient outcomes, these platforms enable data-driven decision-making, leading to more personalized and effective care.
* **Reduced Healthcare Costs:** By improving diagnostic accuracy, preventing disease progression, and reducing the need for hospitalizations, these platforms can help reduce overall healthcare costs.
Users consistently report that these platforms improve their ability to manage complex autoimmune cases and provide better care to their patients. Our analysis reveals these key benefits: faster time to diagnosis, improved patient satisfaction, and reduced administrative burden.
Comprehensive & Trustworthy Review of Autoimmune Disease Management Platforms
Autoimmune disease management platforms represent a significant advancement in the care of patients with autoimmune conditions. This review provides a balanced perspective on their usability, performance, and overall value.
From a practical standpoint, the user experience is generally positive. Most platforms offer intuitive interfaces and easy-to-navigate features. However, some platforms can be complex to set up and require significant training for both providers and patients.
In terms of performance and effectiveness, these platforms have been shown to improve diagnostic accuracy, enhance patient engagement, and streamline workflow. However, the effectiveness of these platforms depends on the quality of the data they receive and the extent to which they are integrated into clinical practice. We’ve observed that platforms with robust data validation and integration capabilities perform best.
**Pros:**
* **Improved Diagnostic Accuracy:** Platforms with advanced ANA pattern recognition and interpretation tools can significantly improve diagnostic accuracy, especially in complex cases.
* **Enhanced Patient Engagement:** Symptom tracking and patient education features empower patients to actively participate in their care, leading to better outcomes.
* **Streamlined Workflow:** ICD-10 code integration and automation features reduce administrative burden and improve billing accuracy.
* **Data-Driven Decision-Making:** Access to comprehensive data on disease activity and treatment response enables more personalized and effective care.
* **Improved Access to Care:** Telemedicine integration expands access to specialists and improves convenience for patients.
**Cons/Limitations:**
* **Implementation Costs:** Implementing and maintaining these platforms can be expensive, requiring significant investment in software, hardware, and training.
* **Data Security Concerns:** Platforms that collect and store sensitive patient data must have robust security measures in place to protect against breaches and unauthorized access.
* **Integration Challenges:** Integrating these platforms with existing EHR systems can be complex and time-consuming.
* **Reliance on Technology:** Patients and providers must be comfortable using technology to effectively utilize these platforms. This can be a barrier for some individuals.
This solution is ideally suited for rheumatologists, immunologists, and other healthcare providers who specialize in the diagnosis and treatment of autoimmune diseases. It is also beneficial for patients with autoimmune conditions who are seeking to actively manage their health.
Key alternatives include traditional EHR systems with limited autoimmune disease management capabilities and point-of-care testing solutions. These alternatives may be less expensive but lack the comprehensive features and functionality of dedicated autoimmune disease management platforms.
Overall Verdict: Autoimmune disease management platforms offer significant potential to improve the care of patients with autoimmune conditions. While there are some limitations and challenges associated with their implementation, the benefits generally outweigh the costs. We recommend that healthcare providers carefully evaluate their needs and choose a platform that aligns with their specific requirements.
Insightful Q&A Section
Here are 10 insightful questions related to positive ANA ICD-10, along with expert answers:
1. **Question:** If a patient has a positive ANA but no specific autoimmune diagnosis, which ICD-10 code is most appropriate?
**Answer:** In this scenario, R77.9 (Abnormality of plasma protein) or R79.89 (Other specified abnormal findings of blood chemistry) might be appropriate, depending on the specific clinical context and the provider’s judgment. It’s crucial to document the absence of a definitive diagnosis.
2. **Question:** How does the ANA pattern (e.g., homogeneous, speckled, nucleolar) influence ICD-10 coding?
**Answer:** The ANA pattern itself doesn’t directly dictate the ICD-10 code. However, it guides the clinician’s diagnostic process. Certain patterns are more strongly associated with specific autoimmune diseases. The ICD-10 code will reflect the *diagnosed* condition, not just the pattern.
3. **Question:** Can a positive ANA result due to a drug be coded using ICD-10?
**Answer:** Yes, drug-induced conditions have specific ICD-10 codes. If the positive ANA is determined to be drug-induced, you would use the appropriate code for the specific drug and the resulting condition. For example, if a drug causes lupus, the code for drug-induced lupus would be used.
4. **Question:** What is the role of ICD-10 coding in tracking the prevalence of autoimmune diseases after a positive ANA finding?
**Answer:** ICD-10 codes provide valuable data for epidemiological studies. By tracking the incidence of specific autoimmune disease codes, researchers can monitor trends and identify potential risk factors.
5. **Question:** How frequently should a positive ANA result without a diagnosis be re-evaluated and potentially recoded?
**Answer:** The frequency of re-evaluation depends on the individual patient’s clinical presentation. Generally, a follow-up appointment within 6-12 months is reasonable. If new symptoms develop, earlier re-evaluation is warranted.
6. **Question:** Are there specific ICD-10 codes for conditions that commonly present with a positive ANA, such as Sjögren’s syndrome or systemic sclerosis?
**Answer:** Yes, both Sjögren’s syndrome and systemic sclerosis have specific ICD-10 codes that should be used when these diagnoses are confirmed.
7. **Question:** How does ICD-10 coding differentiate between a positive ANA in a patient with established lupus versus a newly diagnosed case?
**Answer:** The ICD-10 code for lupus would be the same regardless of whether it’s a new or established case. However, additional codes might be used to reflect the stage of the disease, the presence of complications, or the specific manifestations of lupus in that individual.
8. **Question:** What are the implications of inaccurate ICD-10 coding for positive ANA results on healthcare reimbursement?
**Answer:** Inaccurate coding can lead to denied claims or underpayment for services. It’s essential to use the most specific and accurate code to ensure proper reimbursement.
9. **Question:** Can ICD-10 codes be used to track the effectiveness of different treatments for autoimmune diseases associated with positive ANA?
**Answer:** Yes, by analyzing ICD-10 codes in conjunction with treatment data, researchers can assess the impact of different therapies on disease progression and patient outcomes.
10. **Question:** How do autoimmune disease management platforms assist with accurate ICD-10 coding for positive ANA cases?
**Answer:** These platforms often incorporate features such as code suggestion engines, clinical decision support tools, and integrated lab results to help providers select the most appropriate ICD-10 codes.
Conclusion & Strategic Call to Action
In conclusion, understanding the interplay between a positive ANA test and ICD-10 coding is crucial for accurate diagnosis, effective management, and appropriate healthcare resource allocation. While a positive ANA alone doesn’t define a disease, it serves as an important indicator that necessitates further investigation. The correct application of ICD-10 codes ensures that patient data is accurately captured and utilized for research, public health tracking, and reimbursement purposes. We’ve explored the nuances of this relationship and highlighted the role of autoimmune disease management platforms in streamlining this process.
The future of autoimmune disease management will likely involve even more sophisticated integration of data and technology to personalize care and improve patient outcomes. As diagnostic tools and treatment options continue to evolve, so too will the coding systems used to classify these conditions.
Share your experiences with positive ANA results and the diagnostic journey in the comments below. Explore our advanced guide to understanding autoimmune diseases for a deeper dive into related topics. Contact our experts for a consultation on navigating the complexities of autoimmune testing and diagnosis.