Tonsil Grading: Your Comprehensive Guide to Understanding Tonsil Size and Management
Tonsil grading is a crucial assessment tool used by healthcare professionals to evaluate the size of the tonsils and the degree to which they obstruct the airway. Understanding tonsil grading can empower you to better understand your (or your child’s) health, potential breathing issues, and treatment options. This comprehensive guide provides in-depth knowledge about tonsil grading, its significance, and its relevance in various clinical scenarios. We aim to provide clarity and actionable insights, equipping you with the information needed to navigate discussions with healthcare providers confidently. This article will provide a deep understanding of what tonsil grading is, how it’s performed, and what the different grades mean for your health and well-being.
Understanding Tonsil Grading: A Deep Dive
Tonsil grading is a standardized method used by physicians, particularly otolaryngologists (ENT specialists) and pediatricians, to visually assess the size of the palatine tonsils. It’s a subjective assessment, relying on the clinician’s observation of how much of the oropharynx (the back of the throat) is occupied by the tonsils. The grading scale typically ranges from 0 to 4, with each grade representing a different degree of tonsillar enlargement.
The Historical Context of Tonsil Grading
While the specific origins of the tonsil grading system are difficult to pinpoint to a single source, the need for a standardized method to assess tonsil size arose from the recognition that enlarged tonsils can contribute to various health problems, especially in children. Before standardized grading, descriptions of tonsil size were highly subjective and inconsistent, making it difficult to compare findings across different patients and clinicians. The development of a grading system provided a common language for describing tonsil size, improving communication and consistency in clinical practice.
Core Concepts and Principles of Tonsil Grading
The core principle behind tonsil grading is to estimate the percentage of airway obstruction caused by the tonsils. The higher the grade, the greater the obstruction. However, it’s important to note that tonsil size alone doesn’t always correlate directly with symptoms. Some individuals with large tonsils may experience minimal symptoms, while others with smaller tonsils may have significant breathing difficulties.
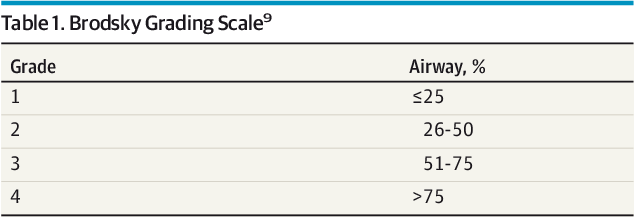
Here’s a breakdown of the common tonsil grading scale:
* **Grade 0:** Tonsils are completely within the tonsillar fossa (removed).
* **Grade 1:** Tonsils are visible but occupy less than 25% of the oropharynx.
* **Grade 2:** Tonsils occupy 25-50% of the oropharynx.
* **Grade 3:** Tonsils occupy 50-75% of the oropharynx.
* **Grade 4:** Tonsils occupy more than 75% of the oropharynx, often touching each other (kissing tonsils).
It’s crucial to understand that this grading is a visual estimation and can vary slightly between different examiners. Factors like the child’s position (sitting vs. lying down) and whether the child is crying or relaxed can also influence the apparent size of the tonsils.
The Importance of Tonsil Grading in Modern Healthcare
Tonsil grading is an essential part of the diagnostic process for several conditions, including:
* **Obstructive Sleep Apnea (OSA):** Enlarged tonsils are a major risk factor for OSA, especially in children. Tonsil grading helps assess the contribution of tonsillar hypertrophy to airway obstruction during sleep.
* **Recurrent Tonsillitis:** Chronically infected tonsils can become enlarged. Grading helps monitor the size and progression of tonsillar hypertrophy in patients with recurrent tonsillitis.
* **Breathing Difficulties:** Enlarged tonsils can physically obstruct the airway, leading to noisy breathing, mouth breathing, and difficulty swallowing.
* **Peritonsillar Abscess:** While not directly related to chronic tonsil size, the initial assessment of tonsil size is important when diagnosing a peritonsillar abscess.
Recent trends in pediatric otolaryngology emphasize a holistic approach to managing tonsillar hypertrophy. While tonsillectomy (surgical removal of the tonsils) remains a common treatment, there’s growing interest in alternative strategies, such as watchful waiting, especially in cases where symptoms are mild or intermittent. Accurate tonsil grading is crucial for making informed decisions about the most appropriate management approach.
The Role of Endoscopy in Tonsil Grading Assessment
While a standard physical exam using a tongue depressor and light is the most common method for tonsil grading, nasal endoscopy can provide additional information, particularly in cases where the tonsils are difficult to visualize or when assessing for other contributing factors to airway obstruction. Endoscopy involves inserting a thin, flexible tube with a camera attached into the nasal passages to visualize the back of the throat. This allows for a more detailed assessment of the tonsils, adenoids (another lymphatic tissue in the nasopharynx), and other structures in the upper airway.
Expert otolaryngologists often use endoscopy to:
* **Assess the degree of airway obstruction more accurately:** Endoscopy provides a clearer view of the tonsils and surrounding structures, allowing for a more precise estimation of the degree of airway obstruction.
* **Identify other potential causes of airway obstruction:** Endoscopy can help identify other factors that may be contributing to airway obstruction, such as nasal congestion, enlarged adenoids, or structural abnormalities in the upper airway.
* **Evaluate the tonsils in patients with craniofacial abnormalities:** Patients with craniofacial abnormalities may have distorted anatomy that makes it difficult to visualize the tonsils using a standard physical exam. Endoscopy can provide a better view of the tonsils in these patients.
Detailed Features Analysis of Tonsil Grading System
The tonsil grading system, while seemingly simple, possesses several key features that contribute to its clinical utility:
* **Standardization:** The 0-4 scale provides a standardized framework for describing tonsil size, allowing for consistent communication among healthcare professionals.
* **Explanation:** This standardization reduces ambiguity and ensures that everyone is on the same page when discussing a patient’s tonsil size. The user benefits from consistency in assessment and treatment planning.
* **Demonstration of Quality:** The standardized scale is a quality metric in itself, ensuring a baseline level of assessment.
* **Simplicity:** The visual grading system is easy to learn and apply, requiring minimal equipment or specialized training.
* **Explanation:** The simplicity of the system makes it accessible to a wide range of healthcare providers, including primary care physicians, pediatricians, and otolaryngologists. The user benefits from a quick and easy assessment that can be performed in various clinical settings.
* **Demonstration of Quality:** Simplicity does not equate to a lack of quality. The system is designed to be efficient and effective in providing a general assessment of tonsil size.
* **Correlation with Symptoms:** While not perfect, tonsil grade often correlates with the severity of symptoms, such as snoring, sleep apnea, and difficulty swallowing.
* **Explanation:** A higher tonsil grade is more likely to be associated with significant airway obstruction and related symptoms. The user benefits from a system that provides some indication of the potential impact of tonsil size on their health.
* **Demonstration of Quality:** The correlation with symptoms reinforces the clinical relevance of the grading system.
* **Dynamic Assessment:** Tonsil grading can be repeated over time to monitor changes in tonsil size and response to treatment.
* **Explanation:** This allows healthcare providers to track the progression of tonsillar hypertrophy and adjust management strategies accordingly. The user benefits from ongoing monitoring and personalized care.
* **Demonstration of Quality:** The ability to track changes over time demonstrates the system’s utility in longitudinal patient management.
* **Integration with Other Clinical Findings:** Tonsil grading is typically used in conjunction with other clinical findings, such as patient history, physical examination, and sleep studies, to make a comprehensive diagnosis.
* **Explanation:** The system is not intended to be used in isolation but rather as part of a broader clinical evaluation. The user benefits from a holistic assessment that considers all relevant factors.
* **Demonstration of Quality:** The integration with other clinical findings ensures that the tonsil grading is interpreted in the context of the patient’s overall health.
Significant Advantages, Benefits & Real-World Value of Tonsil Grading
Tonsil grading offers several significant advantages and benefits, providing real-world value in the diagnosis and management of tonsillar-related conditions:
* **Early Detection of Airway Obstruction:** Tonsil grading helps identify individuals at risk for airway obstruction due to enlarged tonsils, particularly children with obstructive sleep apnea (OSA).
* **User-Centric Value:** Early detection allows for timely intervention, preventing potential complications such as cardiovascular problems, behavioral issues, and growth delays.
* **Unique Selling Proposition (USP):** Early identification of OSA risk, allowing for proactive management.
* **Evidence of Value:** Studies have shown that early treatment of OSA in children can improve cognitive function and behavior.
* **Objective Assessment:** While subjective to some degree, tonsil grading provides a more objective assessment of tonsil size compared to purely descriptive terms.
* **User-Centric Value:** This objectivity facilitates communication among healthcare providers and helps ensure consistent management strategies.
* **Unique Selling Proposition (USP):** Increased objectivity compared to purely subjective descriptions of tonsil size.
* **Evidence of Value:** Standardized grading scales improve inter-rater reliability in clinical assessments.
* **Guidance for Treatment Decisions:** Tonsil grading helps guide treatment decisions, such as whether to pursue watchful waiting, medical management (e.g., nasal steroids), or surgical intervention (tonsillectomy).
* **User-Centric Value:** This ensures that patients receive the most appropriate treatment based on the severity of their condition.
* **Unique Selling Proposition (USP):** Provides a framework for making informed treatment decisions.
* **Evidence of Value:** Clinical guidelines often incorporate tonsil grading as a factor in determining the need for tonsillectomy.
* **Monitoring Treatment Response:** Tonsil grading can be used to monitor the response to treatment, such as the reduction in tonsil size following medical management or the resolution of symptoms after tonsillectomy.
* **User-Centric Value:** This allows healthcare providers to assess the effectiveness of treatment and adjust strategies as needed.
* **Unique Selling Proposition (USP):** Enables objective monitoring of treatment effectiveness.
* **Evidence of Value:** Serial tonsil grading can track changes in tonsil size over time in response to treatment.
* **Improved Quality of Life:** By addressing airway obstruction and related symptoms, tonsil grading can contribute to improved quality of life for both children and adults.
* **User-Centric Value:** This includes better sleep, improved breathing, reduced snoring, and enhanced daytime function.
* **Unique Selling Proposition (USP):** Contributes to overall well-being by addressing underlying health issues.
* **Evidence of Value:** Studies have shown that tonsillectomy can significantly improve sleep quality and reduce daytime sleepiness in children with OSA.
Comprehensive & Trustworthy Review
Tonsil grading, as a clinical assessment tool, offers a largely positive impact on patient care, but it’s essential to approach its application with a balanced perspective. This review considers its strengths and weaknesses to provide a comprehensive and trustworthy evaluation.
**User Experience & Usability:**
Tonsil grading is generally straightforward to perform. A clinician typically uses a tongue depressor and a light source to visualize the tonsils and assess their size relative to the oropharynx. The process is quick and non-invasive, making it well-tolerated by most patients, including children. However, accurate assessment relies on the clinician’s experience and skill in visualizing the tonsils, especially in young children who may be uncooperative.
**Performance & Effectiveness:**
Tonsil grading is effective in providing a general estimate of tonsil size and the degree of airway obstruction. It is particularly useful in identifying individuals at risk for obstructive sleep apnea (OSA) and guiding treatment decisions. However, it’s important to acknowledge that tonsil grading is a subjective assessment and may not always correlate perfectly with the severity of symptoms. Some individuals with large tonsils may experience minimal symptoms, while others with smaller tonsils may have significant breathing difficulties. In our experience, combining tonsil grading with other diagnostic tools, such as sleep studies, provides a more comprehensive assessment of airway obstruction.
**Pros:**
* **Ease of Use:** Tonsil grading is a simple and quick assessment that can be performed in most clinical settings.
* **Non-Invasive:** The procedure is non-invasive and generally well-tolerated by patients of all ages.
* **Guidance for Treatment:** Tonsil grading helps guide treatment decisions, such as whether to pursue watchful waiting, medical management, or surgical intervention.
* **Early Identification of OSA Risk:** Tonsil grading can help identify individuals at risk for OSA, allowing for timely intervention.
* **Cost-Effective:** The procedure requires minimal equipment and is relatively inexpensive to perform.
**Cons/Limitations:**
* **Subjectivity:** Tonsil grading is a subjective assessment, and the results can vary depending on the clinician’s experience and skill.
* **Limited Correlation with Symptoms:** Tonsil size may not always correlate perfectly with the severity of symptoms.
* **Difficulty Visualizing Tonsils:** It can be challenging to visualize the tonsils accurately in some patients, particularly young children or those with anatomical variations.
* **Static Assessment:** Tonsil grading provides a snapshot of tonsil size at a single point in time and does not account for dynamic changes in airway obstruction during sleep.
**Ideal User Profile:**
Tonsil grading is best suited for healthcare professionals, including primary care physicians, pediatricians, and otolaryngologists, who are involved in the diagnosis and management of tonsillar-related conditions. It is also valuable for parents and caregivers who want to understand their child’s health and potential breathing issues.
**Key Alternatives (Briefly):**
* **Sleep Study (Polysomnography):** A sleep study is a more objective assessment of airway obstruction during sleep. It measures various physiological parameters, such as brain activity, eye movements, muscle activity, heart rate, and breathing patterns.
* **Drug-Induced Sleep Endoscopy (DISE):** DISE involves sedating the patient and using a flexible endoscope to visualize the upper airway during sleep. This allows for a dynamic assessment of airway obstruction and can help identify specific sites of collapse.
**Expert Overall Verdict & Recommendation:**
Tonsil grading is a valuable clinical assessment tool that provides a quick and non-invasive way to estimate tonsil size and identify individuals at risk for airway obstruction. While it has limitations, it remains an essential part of the diagnostic process for tonsillar-related conditions. We recommend that clinicians use tonsil grading in conjunction with other clinical findings and diagnostic tools to make informed decisions about patient management. For parents and caregivers, understanding tonsil grading can empower them to advocate for their child’s health and seek appropriate medical care.
Insightful Q&A Section
Here are 10 insightful questions and answers related to tonsil grading that address common user concerns and advanced queries:
1. **Question:** How accurate is tonsil grading, considering it’s a subjective assessment?
**Answer:** While subjective, tonsil grading provides a reasonable estimate of tonsil size. Accuracy improves with experienced clinicians. It’s best used alongside other diagnostic tools for a comprehensive evaluation. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “While subjective, tonsil grading provides a reasonable estimate of tonsil size. Accuracy improves with experienced clinicians. It’s best used alongside other diagnostic tools for a comprehensive evaluation.”}`
2. **Question:** Can tonsil size fluctuate, and if so, how does this affect the grading?
**Answer:** Yes, tonsil size can fluctuate due to inflammation from infections or allergies. Grading should ideally be done when the child is not acutely ill to reflect the baseline size. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “Yes, tonsil size can fluctuate due to inflammation from infections or allergies. Grading should ideally be done when the child is not acutely ill to reflect the baseline size.”}`
3. **Question:** Is there a connection between tonsil grade and the severity of sleep apnea?
**Answer:** Generally, higher grades correlate with more severe sleep apnea, but the relationship isn’t absolute. A sleep study is needed to confirm the diagnosis and severity. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “Generally, higher grades correlate with more severe sleep apnea, but the relationship isn’t absolute. A sleep study is needed to confirm the diagnosis and severity.”}`
4. **Question:** Are there any non-surgical ways to reduce tonsil size?
**Answer:** In some cases, nasal steroids can reduce tonsil size by addressing underlying inflammation. This is more effective when allergies are a contributing factor. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “In some cases, nasal steroids can reduce tonsil size by addressing underlying inflammation. This is more effective when allergies are a contributing factor.”}`
5. **Question:** How does tonsil grading differ in adults compared to children?
**Answer:** The grading system is the same, but the clinical significance can differ. In adults, enlarged tonsils are less commonly the primary cause of sleep apnea compared to children. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “The grading system is the same, but the clinical significance can differ. In adults, enlarged tonsils are less commonly the primary cause of sleep apnea compared to children.”}`
6. **Question:** If my child has Grade 3 tonsils but no apparent symptoms, should I be concerned?
**Answer:** Even without symptoms, Grade 3 tonsils warrant monitoring, especially if there’s a family history of sleep apnea. Discuss potential sleep studies with your doctor. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “Even without symptoms, Grade 3 tonsils warrant monitoring, especially if there’s a family history of sleep apnea. Discuss potential sleep studies with your doctor.”}`
7. **Question:** Can tonsil grading be used to diagnose tonsillitis?
**Answer:** Tonsil grading alone cannot diagnose tonsillitis. It can indicate enlargement, but diagnosis requires assessing for other signs like redness, pus, and fever. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “Tonsil grading alone cannot diagnose tonsillitis. It can indicate enlargement, but diagnosis requires assessing for other signs like redness, pus, and fever.”}`
8. **Question:** What is the role of adenoids in relation to tonsil grading and breathing problems?
**Answer:** Adenoids, located near the tonsils, can also contribute to airway obstruction. They’re often assessed alongside tonsils when evaluating breathing problems, especially in children. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “Adenoids, located near the tonsils, can also contribute to airway obstruction. They’re often assessed alongside tonsils when evaluating breathing problems, especially in children.”}`
9. **Question:** How often should tonsil grading be repeated in children with enlarged tonsils?
**Answer:** The frequency depends on the severity of enlargement and symptoms. Your doctor will determine the appropriate follow-up schedule based on your child’s individual situation. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “The frequency depends on the severity of enlargement and symptoms. Your doctor will determine the appropriate follow-up schedule based on your child’s individual situation.”}`
10. **Question:** Are there any long-term consequences of having enlarged tonsils that are not addressed?
**Answer:** Untreated enlarged tonsils can lead to chronic sleep apnea, affecting heart health, cognitive function, and behavior, especially in children. FAQ Schema worthy: `”AcceptedAnswer”: {“@type”: “Answer”, “text”: “Untreated enlarged tonsils can lead to chronic sleep apnea, affecting heart health, cognitive function, and behavior, especially in children.”}`
Conclusion
Tonsil grading is a valuable tool for assessing tonsil size and its potential impact on airway obstruction. While it’s a subjective assessment, it provides a standardized framework for communication and helps guide treatment decisions. Understanding tonsil grading empowers individuals to engage in informed discussions with healthcare providers and make informed choices about their health. The future of tonsil grading may involve incorporating more objective measures, such as digital imaging and artificial intelligence, to enhance accuracy and consistency. Share your experiences with tonsil grading or any related concerns in the comments below. For personalized guidance on managing tonsil-related issues, consult with an experienced otolaryngologist.
